Latest post
Post Categories
- No categories
Anal Fistula Treatment in Hyderabad
Anal Fistula Management: Understanding, Treatment, and Recovery
Learn about effective strategies for Anal Fistula Management, including surgical and non-surgical treatment options, recovery tips, and FAQs. Find expert insights and comprehensive guidance on this condition
Introduction to Anal Fistula Management
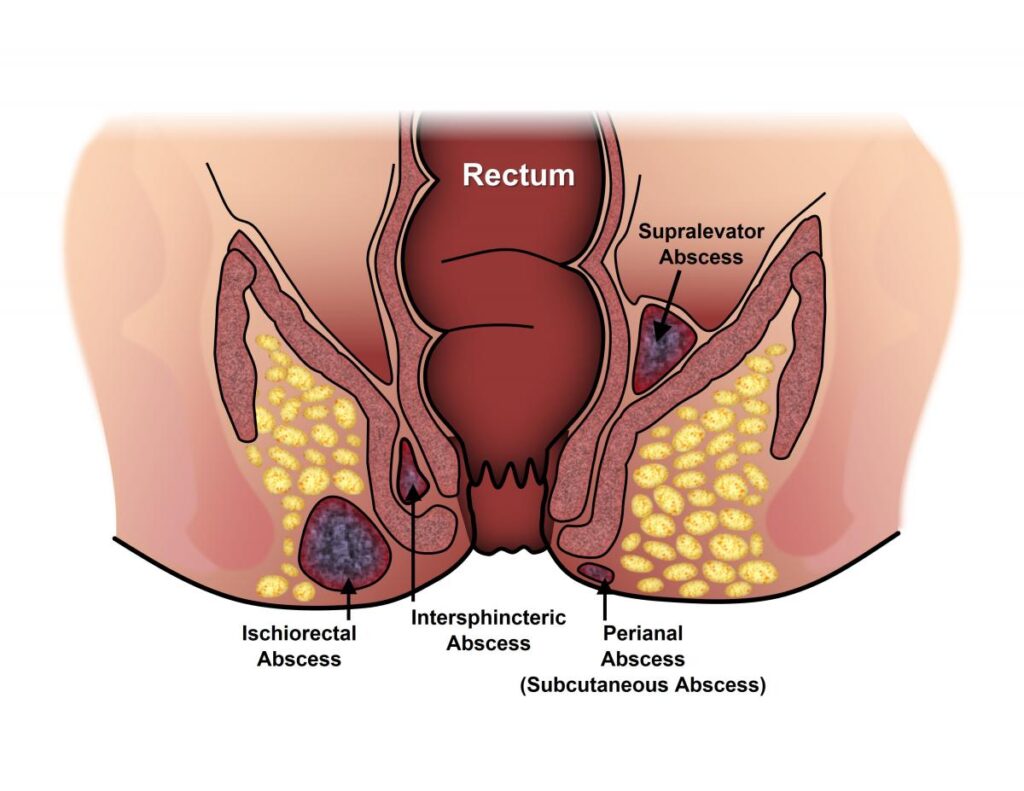
Anal fistulas are abnormal passageways that develop between the anal canal or rectum and the skin around the anus. They often result from an infection in an anal gland and can cause discomfort, pain, and drainage of pus. Managing anal fistulas requires a comprehensive approach that addresses both the underlying cause and the symptoms. In this article, we’ll explore the various aspects of anal fistula management, including treatment options, recovery, and frequently asked questions.
Understanding Anal Fistulas
Anal fistulas can vary in severity and complexity, ranging from simple, superficial tracts to complex networks involving multiple openings and surrounding tissue. Understanding the anatomy and pathophysiology of anal fistulas is crucial for effective management. Key factors include the location of the fistula, the presence of underlying conditions such as Crohn’s disease, and the potential for recurrence.
Diagnostic Evaluation
Accurate diagnosis is essential for determining the most appropriate treatment approach for anal fistulas. Diagnostic tests may include physical examination, imaging studies such as MRI or endoanal ultrasound, and occasionally, examination under anesthesia. These tests help identify the extent of the fistula, any associated abscesses or secondary tracts, and underlying factors that may influence treatment decisions.
Non-Surgical Treatment Options
In some cases, anal fistulas may be managed conservatively with non-surgical interventions. These may include:
- Antibiotics: Used to treat underlying infections and reduce inflammation.
- Fistula Plugs: Synthetic plugs inserted into the fistula tract to promote healing.
- Seton Placement: Placement of a special thread (seton) to drain the fistula and prevent abscess formation.
- Fistulotomy: Cutting open the fistula tract to allow it to heal from the inside out.
Surgical Treatment Options
When non-surgical treatments are ineffective or inappropriate, surgical intervention may be necessary. Surgical options for anal fistula management include:
- Fistulotomy: Surgical cutting of the fistula tract to promote drainage and healing.
- LIFT Procedure (Ligation of Intersphincteric Fistula Tract): Closure of the internal opening and removal of the fistula tract.
- Advancement Flap Repair: Using nearby tissue to cover and seal the fistula tract.
- Fistula Excision and Primary Repair: Complete removal of the fistula tract followed by closure of the wound.
Postoperative Care and Recovery
Recovery from anal fistula surgery depends on the type and complexity of the procedure. Patients may experience discomfort, swelling, and drainage following surgery. It’s essential to follow postoperative care instructions carefully, including wound care, pain management, and dietary recommendations. Most patients can resume normal activities within a few weeks, but full recovery may take several months.
Lifestyle Modifications and Prevention
Making certain lifestyle modifications can help prevent recurrence of anal fistulas and promote overall anal health. These may include:
- Maintaining good hygiene: Keeping the anal area clean and dry to prevent infection.
- Dietary changes: Consuming a high-fiber diet to promote regular bowel movements and reduce strain during defecation.
- Avoiding constipation: Staying hydrated and incorporating physical activity into your daily routine to prevent constipation
Frequently Asked Questions (FAQs) about Anal Fistula Management
Anal fistulas often develop as a result of an infection in an anal gland, which leads to the formation of an abnormal tract between the anal canal or rectum and the skin around the anus.
Diagnosis of anal fistulas typically involves a combination of physical examination, imaging studies such as MRI or endoanal ultrasound, and occasionally, examination under anesthesia.
Yes, non-surgical treatments for anal fistulas may include antibiotics, fistula plugs, seton placement, and fistulotomy.
Surgical options for anal fistula management include fistulotomy, LIFT procedure, advancement flap repair, and fistula excision and primary repair.
Recovery from anal fistula surgery depends on the type and complexity of the procedure but may involve discomfort, swelling, and drainage. Patients are typically advised to follow postoperative care instructions carefully for optimal healing.
Preventing recurrence of anal fistulas involves maintaining good hygiene, consuming a high-fiber diet, avoiding constipation, and seeking prompt treatment for any underlying conditions.
Conclusion
Effective management of anal fistulas requires a tailored approach that addresses the individual needs and circumstances of each patient. By understanding the underlying causes, exploring treatment options, and adopting preventive measures, individuals can optimize their outcomes and maintain overall anal health