Latest post
Post Categories
- No categories
Fecal incontinence Treatment in Hyderabad
Introduction
Fecal incontinence, a condition marked by the involuntary passage of fecal material, poses significant challenges to patients’ quality of life. This article explores various aspects of managing fecal incontinence comprehensively, emphasizing the importance of a multidisciplinary approach to address its complex nature.
Understanding Fecal Incontinence
Fecal incontinence, often termed as bowel or anal incontinence, refers to the inability to control bowel movements, leading to involuntary leakage of stool. It can result from various underlying factors, including muscle damage, nerve dysfunction, or anatomical abnormalities.
Anal Physiology
The anus, a crucial component of the digestive system, plays a pivotal role in fecal continence. Understanding its anatomy and physiological mechanisms is essential for evaluating and managing fecal incontinence effectively.
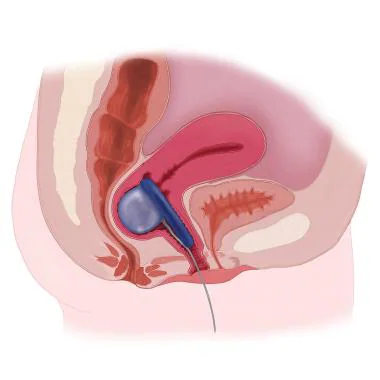
Anatomy and Function of the Anus
The anus comprises complex structures, including internal and external sphincters, pelvic floor muscles, and nerve endings. Coordination between these components facilitates fecal continence by controlling the passage of stool.
Radiology
Diagnostic imaging techniques are instrumental in identifying structural abnormalities and evaluating the underlying causes of fecal incontinence. Radiological examinations provide valuable insights into anatomical anomalies and aid in treatment planning.
Diagnostic Imaging Techniques
Radiological modalities such as MRI, CT scans, and defecography offer detailed assessments of pelvic anatomy and function. These imaging studies help clinicians visualize abnormalities in the rectum, anal canal, and surrounding structures.
Physical Therapy
Physical therapy interventions play a crucial role in rehabilitating pelvic floor muscles and improving bowel control among patients with fecal incontinence. Targeted exercises and therapeutic modalities contribute to enhancing muscle strength and coordination.
Rehabilitation Approaches
Pelvic floor exercises, biofeedback training, and electrical stimulation are common techniques employed in physical therapy for fecal incontinence management. These interventions aim to optimize muscle function and restore continence.
Gynecology
Fecal incontinence presents unique considerations in female patients, necessitating specialized approaches within the realm of gynecology. Understanding the interplay between gynecological factors and fecal continence is vital for tailored management.
Considerations in Female Patients
Gynecological conditions such as obstetric trauma and pelvic organ prolapse can contribute to fecal incontinence in women. Comprehensive evaluation and treatment strategies address both gynecological and continence-related issues.
Urology
Fecal incontinence can impact urinary function, highlighting the interconnectedness of bowel and bladder control mechanisms. Urological evaluation is essential to address potential bladder dysfunction and optimize overall continence outcomes.
Impact on Urinary Function
Neurological conditions affecting bowel control may also influence bladder function, leading to urinary incontinence. Collaborative management involving urologists ensures comprehensive assessment and treatment of pelvic floor disorders.
Digestive System Implications
Conditions such as chronic diarrhea, inflammatory bowel disease, and constipation can exacerbate fecal incontinence symptoms. Gastroenterologists employ a holistic approach to address gastrointestinal issues and enhance continence outcomes.
Colorectal Surgery
Surgical interventions may be necessary for patients with refractory or complex fecal incontinence cases. Colorectal surgeons offer expertise in various surgical techniques aimed at restoring fecal continence and improving quality of life.
Surgical Options
Sphincteroplasty, sacral nerve modulation, and artificial sphincter placement are among the surgical options available for fecal incontinence management. These
procedures are tailored to individual patient needs and aim to optimize continence function.
Multidisciplinary Approach
A multidisciplinary care model is crucial for addressing the diverse needs of patients with fecal incontinence. Collaborative efforts among healthcare professionals ensure comprehensive assessment, personalized treatment plans, and holistic management.
Coordinated Care Strategies
Multidisciplinary teams comprising gastroenterologists, colorectal surgeons, physical therapists, and other specialists collaborate to provide integrated care. This approach facilitates comprehensive evaluation, individualized interventions, and improved patient outcomes.
Case Studies
Real-life case studies illustrate the practical application of multidisciplinary approaches in managing fecal incontinence. These scenarios highlight the effectiveness of coordinated care strategies and showcase successful outcomes for patients.
Conclusion
Fecal incontinence necessitates a multidisciplinary approach to address its multifaceted nature effectively. By integrating expertise from various specialties, healthcare providers can identify primary causes, implement least invasive interventions, and achieve long-term solutions, thereby optimizing patient care and quality of life.
Frequently Asked Questions (FAQs)
Conclusion
Fecal incontinence requires a comprehensive, multidisciplinary approach to identify its primary cause and implement effective management strategies. By integrating expertise from various medical disciplines, healthcare providers can offer personalized care and improve patient outcomes.