Latest post
Post Categories
- No categories
Pelvic Floor Dysfunction Treatment in Hyderabad
Learn about the diverse impact and management of pelvic floor dysfunction, a complex condition affecting bowel function, continence, and perineal pain.
Introduction
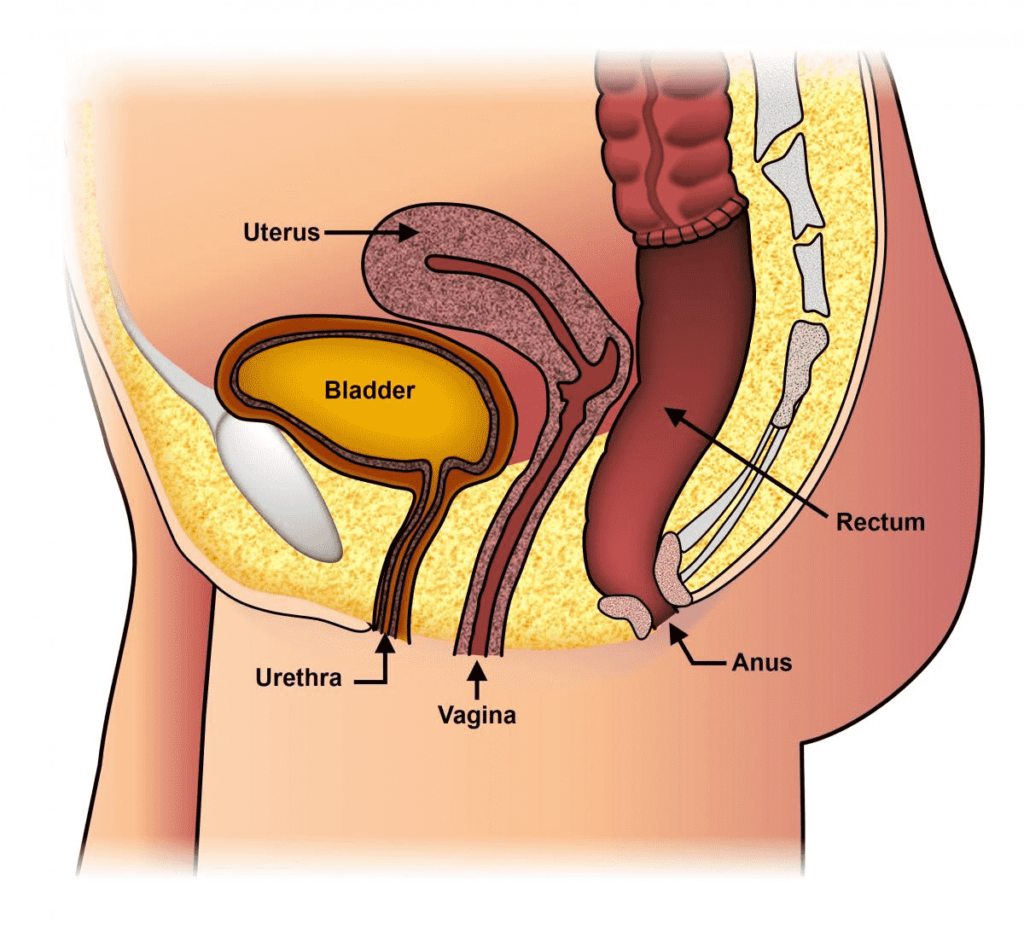
Pelvic floor dysfunction encompasses a range of conditions that affect defecation, bowel storage, continence, and perineal pain. This comprehensive guide explores the causes, evaluation, and management of this multifaceted condition.
Understanding Pelvic Floor Dysfunction
Pelvic floor dysfunction is a complex condition resulting from various factors such as childbirth, obesity, radiation, surgery, or pelvic trauma. It affects both sexes and often involves the coexistence of multiple disorders.
Impact on Bowel Function
Pelvic floor dysfunction can significantly disrupt normal bowel function, leading to symptoms such as constipation, diarrhea, or incomplete evacuation.
Continence Issues
Individuals with pelvic floor dysfunction may experience difficulties with urinary or fecal continence, impacting their quality of life and emotional well-being.
Causes and Risk Factors
Understanding the underlying causes and risk factors of pelvic floor dysfunction is crucial for effective management.
Childbirth
Childbirth, especially vaginal delivery, can weaken the pelvic floor muscles and contribute to dysfunction later in life.
Surgery or Trauma
Pelvic surgeries or trauma involving the pelvic region can damage the muscles and nerves, leading to dysfunction.
Evaluation and Diagnosis
A multidisciplinary approach is essential for accurately evaluating and diagnosing pelvic floor dysfunction.
Comprehensive Assessment
Evaluation includes a thorough medical history, physical examination, and diagnostic.
Symptom Definition
Defining the patient’s symptoms is crucial for tailoring effective treatment strategies and improving their quality of life.
Treatment Approaches
Managing pelvic floor dysfunction requires a personalized approach addressing the underlying causes and symptoms.
Pelvic Floor Exercises
Pelvic floor muscle training, such as Kegel exercises, can strengthen weakened muscles and improve symptoms.
Dietary Modifications
Dietary changes, including increased fiber intake and adequate hydration, can alleviate constipation and improve bowel function.
Behavioral Therapies
Behavioral therapies, such as biofeedback or bowel retraining, help patients regain control over their pelvic floor muscles and bowel function.
Frequently Asked Questions (FAQs)
Common symptoms include constipation, fecal or urinary incontinence, pelvic pain, and discomfort during bowel movements.
While pelvic floor dysfunction affects both sexes, it is more commonly reported in women due to factors such as childbirth and hormonal changes.
While pelvic floor dysfunction may not be completely cured, it can be effectively managed with a combination of lifestyle modifications, therapies, and sometimes surgical interventions.
In some cases, surgical interventions such as pelvic floor repair or nerve stimulation may be recommended for severe or refractory cases of pelvic floor dysfunction.
Consulting with a healthcare provider specializing in pelvic floor disorders, such as a urologist, colorectal surgeon, or urogynecologist, is recommended for proper
evaluation and management.
Yes, pelvic floor dysfunction can impact sexual function, leading to discomfort or pain during intercourse. However, addressing underlying pelvic floor issues can often improve sexual function.
Conclusion
Pelvic floor dysfunction is a complex condition with diverse symptoms and underlying causes. By understanding its impact and seeking comprehensive evaluation and management, individuals can effectively address their symptoms and improve their quality of life.