Latest post
Post Categories
- No categories
Rectal Prolapse and internal intussuception Treatment in Hyderabad
Call: +91-7013714402
Addressing Rectal Prolapse and Internal Rectal Intussusception: Evaluation and Management
Explore the initial evaluation, diagnostic work-up, and management options for rectal prolapse and internal rectal intussusception, covering both nonoperative and operative approaches in detail.
Introduction
This chapter delves into the initial evaluation, diagnostic work-up, and management options for rectal prolapse and internal rectal intussusception. Understanding the nuances of these conditions is crucial for devising effective treatment strategies and optimizing patient outcomes.
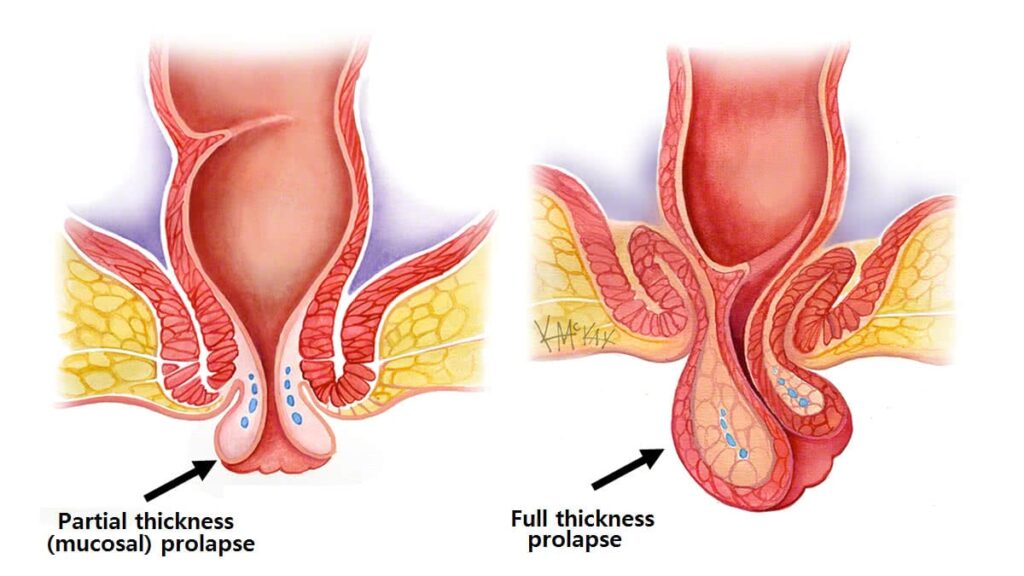
Exploring Rectal Prolapse
Understanding the initial evaluation and diagnostic work-up of rectal prolapse is essential for tailoring appropriate management strategies to each patient’s unique needs.
Clinical Presentation
Rectal prolapse often presents with symptoms such as protrusion of the rectal tissue through the anus, pelvic pressure, and difficulty with bowel movements.
Diagnostic Work-up
The diagnostic work-up typically includes a thorough physical examination, including a rectal exam and assessment of pelvic floor function.
Managing Rectal Prolapse
Effective management of rectal prolapse requires a multimodal approach encompassing both nonoperative and operative interventions.
Nonoperative Management
Nonoperative management may involve lifestyle modifications, pelvic floor exercises, and the use of stool bulking agents to improve bowel function.
Operative Interventions
Surgical management options for rectal prolapse include myriad abdominal and perineal approaches, each associated with distinct advantages and considerations.
Understanding Internal Rectal Intussusception
Internal rectal intussusception presents unique diagnostic and management challenges, particularly in patients with defecatory dysfunction.
Diagnostic Evaluation
The diagnostic work-up of internal rectal intussusception involves specialized tests, including defecography and dynamic pelvic floor MRI, to assess pelvic floor function and rectal anatomy.
Nonoperative Management
In most cases, internal rectal intussusception is managed conservatively, focusing on addressing underlying defecatory dysfunction and optimizing bowel habits.
Comparative Management Strategies
Comparing the management strategies for rectal prolapse and internal rectal intussusception highlights the importance of tailoring treatment to each patient’s specific clinical presentation and underlying pathophysiology.
Nonoperative Versus Operative Management
While rectal prolapse often requires surgical intervention for definitive management, internal rectal intussusception is predominantly managed conservatively, emphasizing the importance of accurate diagnosis and individualized treatment plans.
Frequently Asked Questions (FAQs)
Common symptoms include rectal protrusion, pelvic pressure, and difficulty with bowel movements
Surgery may be necessary for rectal prolapse that significantly impairs quality of life or does not respond to conservative measures.
Internal rectal intussusception is typically diagnosed through specialized tests such as defecography and dynamic pelvic floor MRI.
Yes, internal rectal intussusception is often managed conservatively through lifestyle modifications and pelvic floor exercises
Surgical approaches for rectal prolapse include abdominal procedures such as rectopexy and perineal approaches such as the Delorme procedure
Complications of rectal prolapse surgery may include infection, bleeding, and recurrence of prolapse.
Conclusion
This chapter provides a comprehensive overview of the initial evaluation, diagnostic work-up, and management options for rectal prolapse and internal rectal intussusception. By understanding the complexities of these conditions, healthcare providers can offer tailored treatment plans to optimize patient outcomes.
Contact Us
Book An Appointment!
To schedule a consultation with our expert colorectal surgery team or inquire about
our services, please contact us at:
Address
212, Kokapet Terminal, Gandipet Main Rd, Kokapet, Hyderabad, Telangana 500075
Phone
+91-7013714402
info@colorectalclinic.com